Is it endo, adeno or PCOS?
Do you know the differences between endometriosis, adenomyosis and PCOS? When you’re trying to receive a diagnosis for the symptoms you’re experiencing, it’s important to know which is which. A lot of the symptoms can overlap and often it can be confusing to decipher which symptom is related to which condition. So, let’s break it down and discuss!
Endometriosis
Endometriosis affects approximately one in ten people assigned female at birth (Zondervan, Becker & Missmer, 2020). It is a condition where tissue similar to that of the lining of the uterus (the endometrium) implants or grows elsewhere within the body, most commonly in the pelvic cavity (uterus, ovaries, bladder or bowel). It is also important to note that endometriosis has also now been found within every organ of the body (Weyl, et al., 2021).
Adenomyosis
Adenomyosis is a disease where the lining of the uterus (the endometrium) grows into the muscle of the uterus (the myometrium). Sufferers of adenomyosis experience numerous microscopic bleeds in the muscle wall of the uterus, during the menstrual phase of their cycle (Vannuccini & Petraglia, 2019).
PCOS
Polycystic ovarian syndrome affects approximately one in ten people assigned female at birth (Escobar-Morreale, 2018). It is characterised by high levels of androgens, polycystic ovaries and oligo or anovulation. As it is a ‘syndrome’ it is a collection of symptoms (Boyle & Teedle, 2012). It is also important to note that despite the name ‘polycystic ovary syndrome’, polycystic ovaries are not necessarily required to have PCOS.
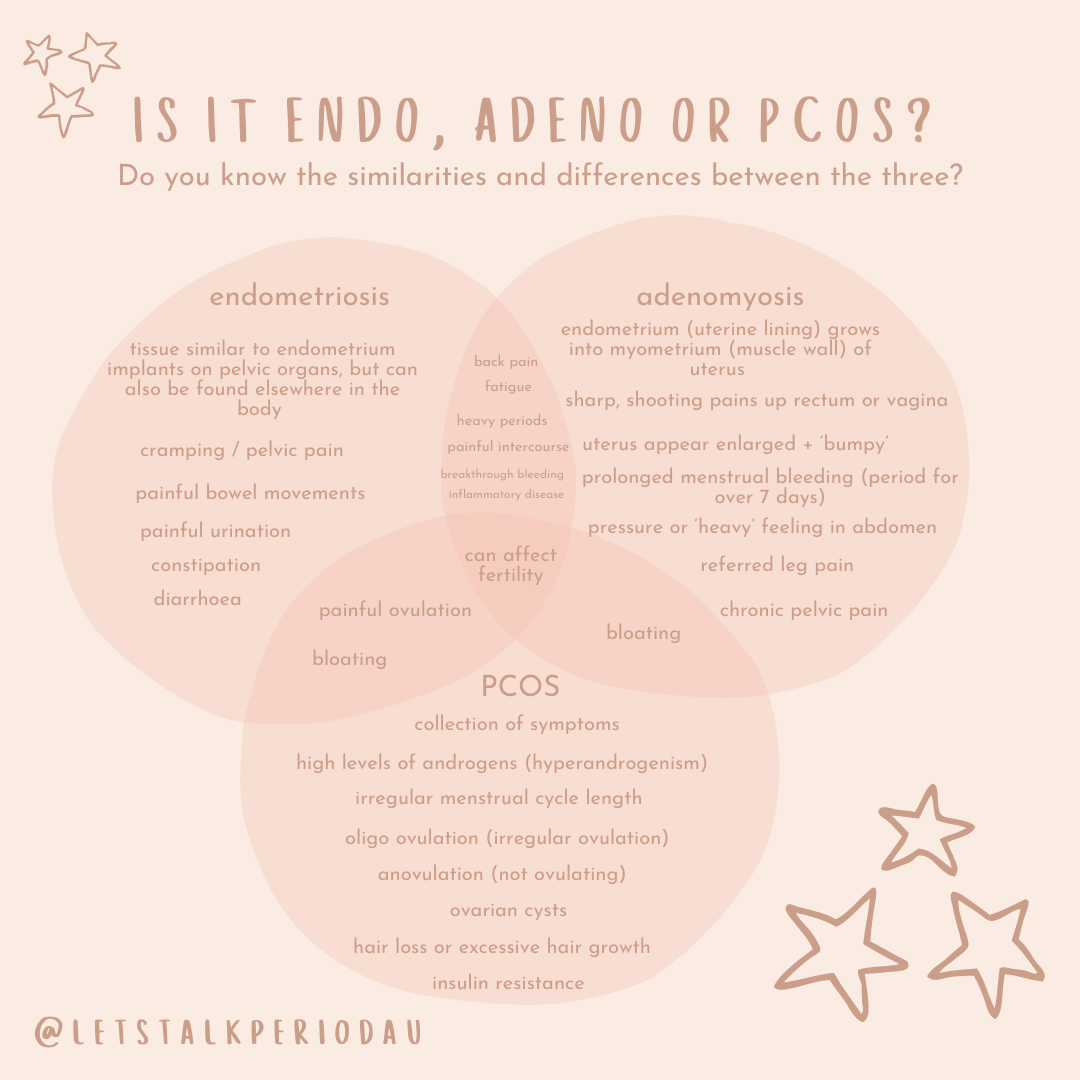
Now we know the overall definition of each condition, let’s take a closer look at the symptoms of each and how endo, adeno and PCOS share similarities, but also differences too! I find graphics super helpful, so this Venn diagram below showcases the different symptoms for each condition, as well as those which overlap. Alternatively, the list of symptoms for each condition is listed below too, as well as diagnostic criteria too.
It’s also important to note that each person is different, and not everyone will have exactly the same symptoms or experience every single symptom associated with a specific condition. If you experience symptoms from all three conditions, it’s important to note which other symptoms you may also be experiencing exclusively. Keeping track of these can assist in early diagnosis and effective interventions. You may find using an app or symptom tracker helpful.
Endometriosis Symptoms
heavy periods
breakthrough bleeding (bleeding which occurs between menstrual periods)
cramping / pelvic pain
back pain
painful intercourse
painful bowel movements
painful urination
painful ovulation
constipation and/ or diarrhoea
bloating
fatigue
fertility can be affected (recurrent miscarriages, trouble conceiving)
Diagnostic: presence of endometrial lesions seen via laparoscopy and confirmed via histology, ultrasound can assist in identifying deep infiltrating endometriosis, endometriomas and possible adhesions, however it is unable to determine the presence of superficial endometriosis.
Adenomyosis Symptoms
heavy periods
prolonged menstrual bleeding (period lasting over seven (7) days
breakthrough bleeding (bleeding which occurs between menstrual periods)
sharp, shooting pains up rectum or vagina
pressure or heavy feeling in abdomen
painful intercourse
chronic pelvic pain
back pain
referred leg pain
bloating
fatigue
fertility can be affected (recurrent miscarriages, trouble conceiving)
Diagnostic: uterus appears inflamed, bumpy, ‘bulky’ and tubal thickening is seen via laparoscopy. Additionally a greater junctional zone (the zone between the the endometrium and myometrium) is evident on MRI, or increased vascularity (blood flow), myometrium thickening and difficulty clarifying the endometrium and myometrium border on ultrasound can indicate adenomyosis
PCOS Symptoms
high levels of androgens (hyperandrogenism)
irregular menstrual cycle length
oligo-ovulation (irregular ovulation)
an-ovulation (ovulation is not occuring)
painful ovulation
ovarian cysts
heavy periods (where cycle length has been extended and endometrium has continued to thicken)
bloating
hair loss or excessive hair growth
acne
insulin resistance
difficulties with weight maintenance
fertility can be affected (recurrent miscarriages, trouble conceiving)
Diagnostic: Rotterdam criteria is used as the gold standard of diagnosis. Two out of three criteria would be present to form a diagnosis of PCOS. These include; hyperandrogenism (high levels of testosterone) via pathology results from a blood test, oligo/anovulation which is evidenced by irregular or abnormally long menstrual cycle lengths and polycystic ovaries present on ultrasound.
References
Boyle, T. & Teede, H.J. (2012). Polycystic ovary syndrome: an update. Reproductive Health, 41(10), 752-756. https://www.racgp.org.au/afp/2012/october/polycystic-ovary-syndrome/
Escobar-Morreale, H.F. (2018). Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nature Reviews Endocrinology, 14(5), 270-284. http://dx.doi.org.ezp01.library.qut.edu.au/10.1038/nrendo.2018.24
Vannuccini, S. & Petraglia, F. (2019). Recent advances in understanding and managing adenomyosis. F1000 Research, 283, 1-10. https://doi.org/10.12688/f1000research.17242.1
Weyl, A., Illac, C., Delchier, M.C., Suc, B., Cuellar, E. & Chantalat, E. (2021). Splenic lesion mimicking breast metastasis: the first description of splenic parenchymal endometriosis. Journal of Endometriosis and Pelvic Pain Disorders, 13(1), 69-73. https://doi.org/10.1177/2284026520960846
Zondervan, K.T., Becker, C.M. & Missmer, S.A. (2020). Endometriosis. New England Journal of Medicine, 382(13), 1244-1256. https://doi.org/10.1056/NEJMra1810764
Disclaimer: Content on Let’s Talk, Period. is produced for educational purposes only, and the information, recommendations and topics discussed throughout does not constitute medical advice, nor does it take into consideration your personal circumstances or medical history. This content should not be used in place of tailored advice and treatment from your personal medical team, nor is it designed to treat or diagnose any medical condition/s. Let’s Talk, Period. and all contributors for Let’s Talk, Period. accept no responsibility or liability for any expenses, damages, losses or costs you or any other party may incur as a result of the content shared across any Let’s Talk, Period. platform.